Designing therapeutic environments for residential aged care

Q: How can we design for radical inclusion in residential aged care?
A: By creating environments that are enabling and empowering for people by designing to include residential aged care in the life of our communities.
Most of us go to residential aged care when we know someone who lives there, but not before or after. People living in residential aged care, and the way their environments are designed, are largely out of sight. There is often discussion about
care and costs in the media, but not about living, and the lives of the people who live there.
We’ve all lived through lockdowns, so we know what it is like to not go out when we wish to, to not be able to do the
things we would like to do, to be told to do things at certain times and have our options curtailed. For many people living in residential aged care this is still their life. And sadly, the community accepts it. It’s OK, for them. We don’t include people living in residential aged care in the goals we set for our lives, and for our community.
Apply the evidence and strong practice base
If we want to design for inclusion in residential aged care, we need to apply the evidence and strong practice base that has been developed over the last four decades. Over this time, frailty levels in aged care have increased significantly and it is estimated that more than two-thirds (68.1%) of aged care residents have moderate to severe cognitive impairment.
Australian and international research has shown that the environment has a key role to play in enabling people to use their abilities as they become frailer and are not able to live independently, due to physical and/or cognitive impairment. The application of a number of design principles has been shown to have a positive impact on the behaviour and quality of life of people living in residential aged care.
In Australia, these principles are the foundation of extensive dementia design training resources used by Dementia
Training Australia, Dementia Australia, and Alzheimer’s WA. They were used to organise and frame the World Alzheimer’s
Report 20201 and are described in the Dignity Manifesto of Design as 10 principles:
- Begin each project by developing a vision for a dignified way of life for people living with dementia.
- Where safety measures are agreed to be appropriate, design them to be as unobtrusive as possible.
- Design the environment to reflect a human scale.
- Plan the environment to make it easy for people to see and move where they want to go.
- Optimise stimulation, so that helpful stimulation is emphasised and unhelpful stimulation is minimised.
- Promote movement, engagement, and meaningfulness.
- Afford people opportunities to enjoy contact with nature.
- Design all components of the environment to be as familiar as possible.
- Afford people opportunities to choose to be alone or with various size groups of people.
- Provide easy access and connection to and from local communities, families, and friends.2
The manifesto seeks to provide an internationally agreed consensus on the values and principles that guide the design
of enabling environments for people living with dementia. Signatories include people living with dementia and their
carers, many eminent experts in design and architecture, and the UN Special Rapporteur on the Rights of Persons with Disabilities. The manifesto takes a stand on what is needed if we are to include people living with dementia in the life of our communities, whether they are living in their own homes or in residential aged care.
Environments that promote wellbeing and quality of life
As architects, we need to create inclusive residential aged care settings that promote wellbeing and quality of life. We need to focus on much more than decoration and furniture and use design to create a familiar environment in every sense, remembering who will live in these places. Residents need an environment that is legible and meaningful to them, not one that showcases the latest architectural trends. This does not preclude great design. It does mean, however, that the focus is on the resident. We also need to give greater emphasis to designing outdoors and going outdoors.
We need to design so it is just as safe to be outside as it is to be inside. We need to think about where outdoor spaces are, and how and why a resident would go there. We need to design environments that support people who live in aged care and the staff who work there. We need to create therapeutic environments that are easily understood and manageable, so people can find their room, and are not left walking up and down a hotel like corridor, searching, because we haven’t paid attention to scale and visual access, because we haven’t paid attention to optimising stimulation, and have instead created environments that lead people to become anxious and sometimes aggressive. This is not good for the resident but is also terrible for staff and for the family.
As part of my PhD research, I have spent weeks sitting in indoor and outdoor social spaces in residential aged care, observing how residents use them, as I explore how we can use design to encourage residents to go outdoors. As architects we need to spend time with people who live and work in residential aged care so we can use their practice knowledge and lived experience to inform our designs. We also need to use the skills we have to help our clients understand the importance of the environment in the lives of residents, staff and families.
Goals, principles, approaches, responses
One way to create a therapeutic environment is to use the schema that was published in the World Alzheimer’s Report 2020. We can start by articulating the goals of the project, and then apply key design principles to achieve these. The next step is to interpret the principles using approaches and responses that are context and people specific. The goals for a project can be described in many ways and are likely to vary for every project and client. We need to encourage clients to articulate a vision, and to think about how people in residential aged care can live, and not simply exist. We need to explore how residential aged care can be part of the wider community, and not isolated and apart from it.
The National Aged Care Design Principles and Guidelines (2024) will be most useful if read with an understanding of the principles contained in the World Alzheimer’s Report 2020. The Commonwealth’s document identifies four key design principles of focus. These are: Enable the Person; Cultivate a Home; Access the Outdoors; and Connect with Community. What if we were to take each of these as a goal and apply the 10 principles to each? That would mean that as we think about access to outdoors, we would think about all the principles, about visual access, scale and stimulation, about meaningful engagement and creating a familiar environment with places for people to be on their own or with others. The potential is enormous when we use these principles to respond to goals, and then in turn use the principles to guide the design’s direction and detail.
The schema described in the World Alzheimer’s Report 2020 is a way to apply the knowledge we have learnt from decades of research and practice in many different
settings. Knowledge can be used in a culturally and contextually appropriate way, rather than taking a cookie-cutter approach where one-size-fits-all and components are selected from a shopping list.
Creating therapeutic environments
Residential aged care is an important part of a community. We need to raise awareness about the importance of the environment in the eyes of the community so that people who make decisions about aged care (and who will live there) realise that the environment matters and know what is important. We also need to encourage providers to spend time (not extra money) creating therapeutic environments, environments that support and enable the people who live and work there. We have a responsibility as a profession and an opportunity to do this. Australia used to be a world leader in aged care design. Let’s reclaim this place.
Residential aged care projects are large projects. But at their heart are the people who live there. That is why they happen, because older people, many of whom will be living with dementia, need care and support to live out their lives. The most important thing we can do to be radically inclusive is to put these people at the heart of our designs.
Kirsty Bennett FRAIA, is the co-author of the World Alzheimer’s Report 2020: Design Dignity Dementia, the founding manager of Dementia Training Australia’s National Design Education Service, a volunteer caregiver, and is undertaking a PhD in design at Swinburne University of Technology. She is a co-founder of the Evoke Collective and Enable Everyone.
Published online:
07 Nov 2024
Source:
Architect Victoria
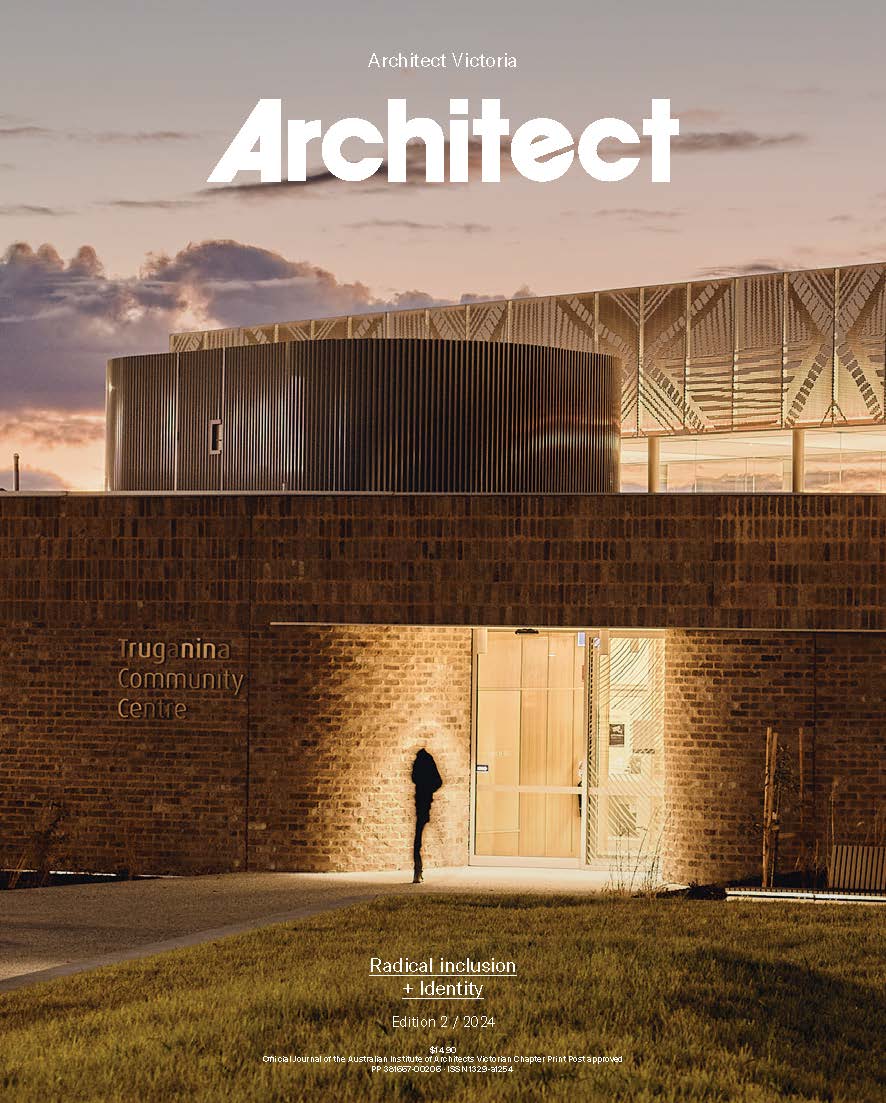
Radical inclusion + Identity
Edition 2 / 2024